There are a few NKH kids right now who are struggling. Who are at home and ill. Who are in hospital on the ward. Who are in hospice, on what the doctors say is towards the end of their lives. It’s hard, being in a virtual community, physically so far away knowing these families are hurting, that these kids are suffering.
There are also many children who have fought their fight with NKH, who have gained their angel wings and are no longer suffering. Their families are still grieving, though. Still hurting.
And I say all these things, but I don’t have words for how deep the suffering is. How truly intense and horrific it is. I don’t have words for that kind of anguish.
I struggle. I don’t have words and I think this is all coming out wrong – how do I talk about this? How do I talk about the tears and the emotions just below the surface? How I’m constantly grappling with how I feel, with grief. Is it a relief for all the children who have passed? Will it be a relief for the children who are suffering right now, considering how much pain and hurt there has been in their lives? Is there relief for their families? Will there one day be relief for us?
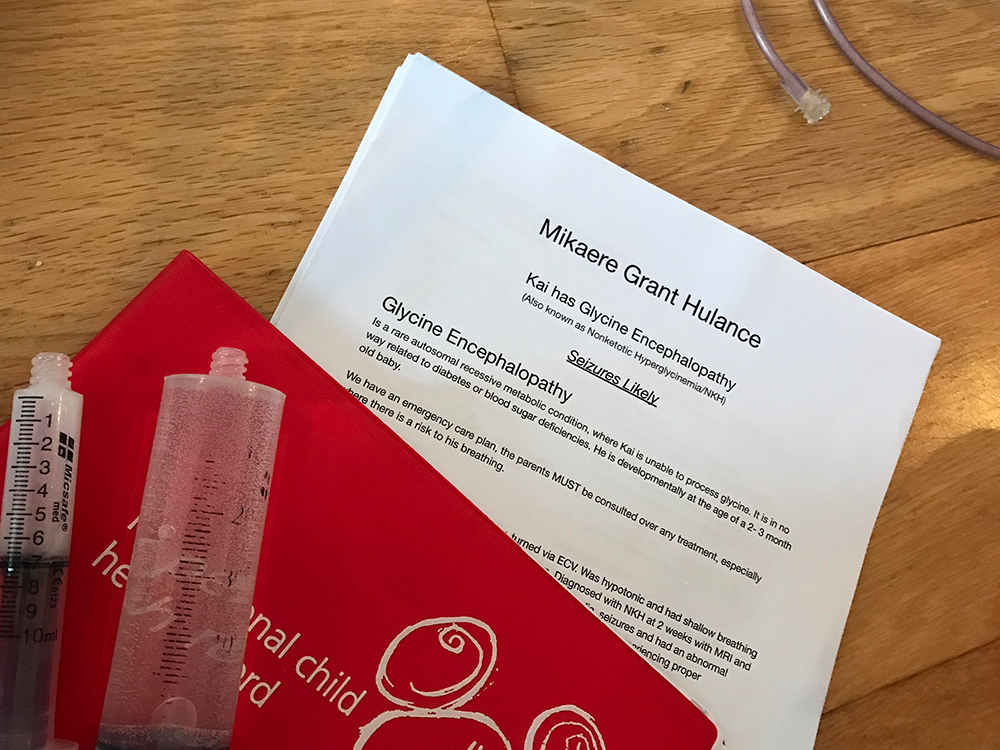
Because that’s the thing, I can’t comprehend Mikaere dying. I can’t. But he will, one day, because NKH is terminal. I don’t want death to visit us. I don’t want death to visit any of the families that are waiting for it right now. I don’t want the curtain of grief to envelop any of our NKH families. I just don’t.
And I feel powerless to help. The families who children have passed, the families that are struggling. I don’t feel I can bring comfort to them. I don’t know how to support them. I send messages to let them know we’re thinking of them (and I am, all day every day) but it feels… inconsequential. I feel powerless to help our little family, and the endless waiting and fear for the terminal end.
There have been a few times we’ve waited for the news. A handful of times we’ve sat, anxiously waiting for that call, to hear when another child gained their angel wings. We’d send love and thoughts and cry. We’d talk about organ failure and seizures and that respiratory arrest is more likely to happen before cardiac arrest. We talk about the dignified death bill, and slower than slow breathing rates. We’re normalising the lead up to death.
I hate that this kind of conversation is normal for us now. That we as parents fight so hard to keep our children happy and healthy, and that we’re powerless in the end to stop the pain and suffering that comes with NKH.
I hate that our days with our kids are tinged with the word terminal. That sometime in our future with Mikaere we’ll be in the same position. That we’ll, one day, be watching his organs fail and be witness to his pain and his suffering. To his death. Just like other NKH families are right now.
I’m heartbroken. I’m absolutely heartbroken.
I’m talking about death and dying today because November 2nd, was NKH Remembrance Day. I’m late by a few days, but I want to pause and remember our NKH kids.
I want remember Alexander, the sweetest little sausage there was. I want to to remember Kaleb, and his cheeky grin.
Gregory, and his brother Elijah who is missing him. Halle Mae. And Cathryn. Maynak. Siem.
There are actually many more children. There’s a list. A list of 124 children who have died from NKH whose names should be remembered. There’s a slide show, even. And I started reading the names… there are so many names. Too many names.
And I’m aware that these names, they’re just the ones in our NKH group. They’re just the ones we know about. Other languages, other countries… they have their own groups with children who are dying before their time. They also probably don’t include the families whose babies died before they could even find support in the NKH groups.
Too many names. Too many children.
I don’t want them to be forgotten. I want to remember them, I want their families to know I remember them. To know their names, and their faces. They made marks, they made a difference. They were loved.
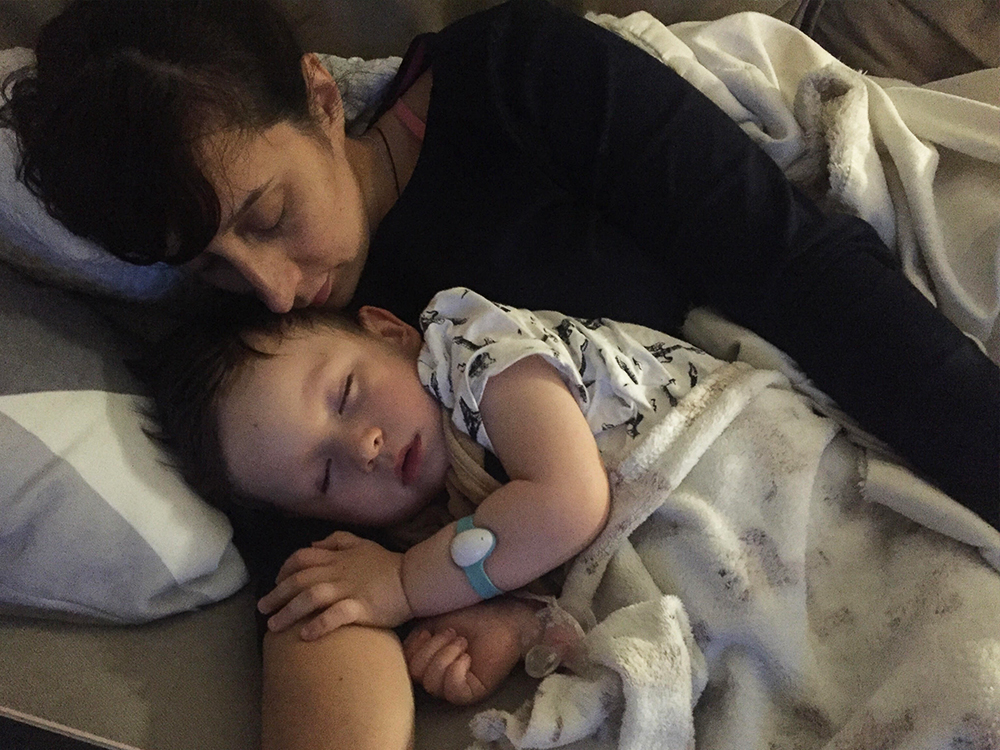
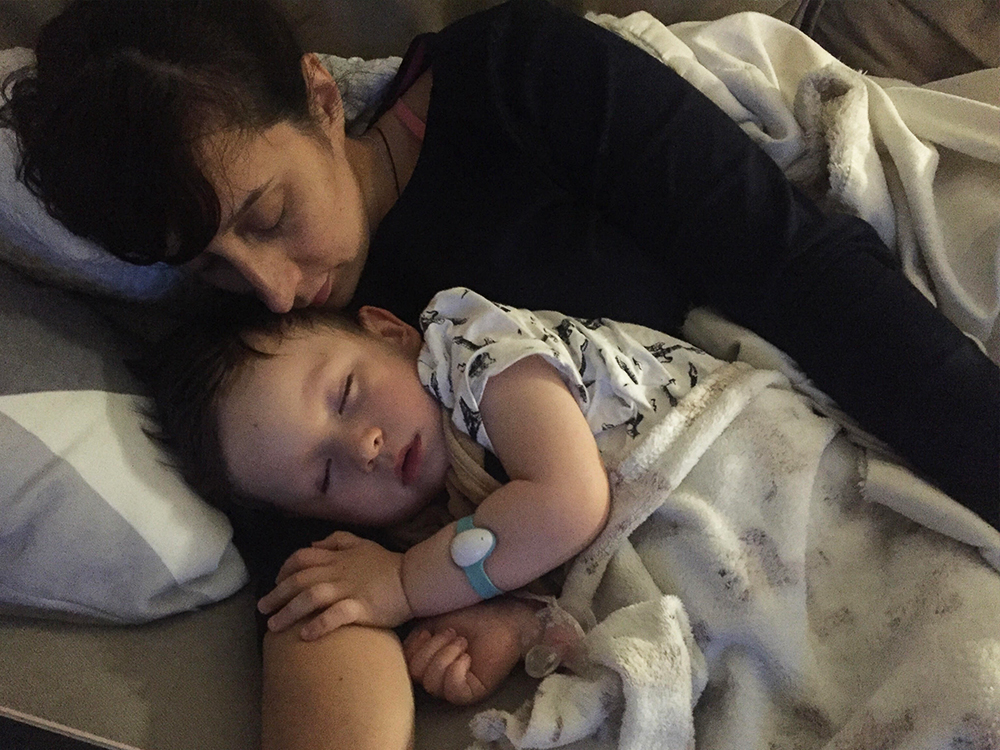
I held my little guy a bit closer today while I remember the others. And I think about how all of those children were so loved like I love my little guy. So loved and cherished. NKH can suck it.