The thing with having a child that can’t be upright by himself means that every time Mikaere is upright, his legs are strapped down. Every time. He’s entire lower half is static. Can you even imagine? That to upright independently, you have to have your entire body from the chest to your toes strapped down.
This means Mikaere has never been in an upright position and realised he has ankles. He’s never had the opportunity to understand what his ankles are, when he’s upright. To realise what his legs are for. Or realised that if he locks his knees he could stand.
There was also a theory, once, that if Mikaere learnt he could move his legs, realised he had mobility and ankles and knees, he might begin to weight bear. Maybe (this is very long long shot).
So I looked around at equipment that might be supportive for his trunk (because obviously he’s going to need support) and have his legs free, and I came across gait trainers, or walkers. They’re exactly like what they sound – exactly like those little walkers you plop babies in so they can move their feet and go – except instead of fisher price it’s a full on piece of therapy equipment.
I convinced our NHS physio that it was a good idea to try, and she said no harm. So we tried a walker. We organised a rep to come out and fit it and put him in it. You guys. Nothing in the sky aligned for us.
Mikaere refused to nap and he’d a load of seizures so already we were on the back foot. Coaxing Mikaere into the walker, sans nap, into a completely new experience was both fine and heartbreaking.
There were moments were he was happy. Holding his head up, curious about what was happening to his legs, the freedom and movement, but when he realised he couldn’t get out of it, he screamed. Big tears, very unhappy, completely helpless, frustrated that what he wanted (out) he couldn’t do himself. Proper, loud, distraught screaming. Back arching, over extension. Rage. Screaming.
I hate it when he screams. I hate it when we’re trying something and we go too fast, or it’s too much and I can’t anticipate it and he just, it’s too much. Screaming. It hits me right in the heart that something I pushed for has caused my baby to scream like that.
I pretty much tore through the straps to get him out out as quick as we could, and comforted. We cuddled and sang songs and coaxed him back in. Fine for a few minutes, not fine after that.
Essentially I called it after the third attempt. My aim was to see if we could put him in a supportive position to teach him how to weight bear through his legs himself. Or even, teach him that his legs are helpful for weight bearing, for standing. To see if he had any inclination in propelling himself forward with his legs. To teach him he has ankles.
Turns out he wasn’t keen. We had a talk about how neurotypical babies learn, but things like a baby doorway bouncer or a baby activity ring, they don’t have enough core support for him. Our NHS physio basically said they wouldn’t fund it. He didn’t show enough forward momentum for him to show that it would be beneficial. Womp.
We talked about standing slings, to see if I could suspend him from a doorway (like a doorway bouncer without the bounce) but the hoist company wouldn’t sell the sling to a family without a hoist. Our plan was to suspend it from a pull up bar in the doorway, knowing full well that if it could hold Sam’s weight it could hold Mikaere’s. But no go. (I did, later, try suspend the upsee vest from the pull upbar, but it makes him lopsided, head forward legs back. Not what I was looking for!)
And so I mulled on it. And thought about it. And then I mentioned to our private physio what I was thinking. See, the difference between our private physio + our NHS physio is that she has the time, and space and freedom to try different things. She isn’t bound by KPI’s, or the weird NHS culture that our other (lovely, completely competent and wonderful) physio is. She’s also knows Mikaere well enough to know what he’s like on a bad day, and how different he is on a good day.
So, we tried again, privately. I’d look at private funding, but first we’d get the rep out and see him again in a walker.
It was 100% a different experience. We went slow. Spending a good few minutes looking at the walker, touching the walker, going in and out of the walker. Feeling his feet, on the carpet, on the tiled floor. Feeling his weight move from the front of his foot, to his heel. Literally holding up his head in our hands, his hands exploring the conveniently placed ring for holding onto.

What a different experience. He didn’t love it, he tolerated it. But – BUT! He was using his ankles, weight was going through his feet. There was definite learning there, figure out how and when and what! If the goal is for him to be more aware of his body, to learn he has ankles and to strengthen those muscles and maybe, one day (extreme stretch goal), weight bear independently, then this session showed he could.
So we pushed go. I got funding, and we said yes please to the rep company, Jiraffe. We would like a small pacer please. In speedy purple. Could we please have a quote? It took a while for the funding come through, but it did (thank you, Elifar!) and when it had, unfortunately Jiraffe had upgraded to a new walker that wasn’t quite as appropriate for Mikaere. They only had the demo walker left.
We’re not precious, so we asked if we could purchase the demo version. There was radio silence on Jiraffe’s end, and when they came back, blow me over with a feather. Because Mikaere’s condition is terminal, they would like to GIFT the demo pacer to Mikaere! Oh my days! We were so grateful, so so so grateful and accepted.
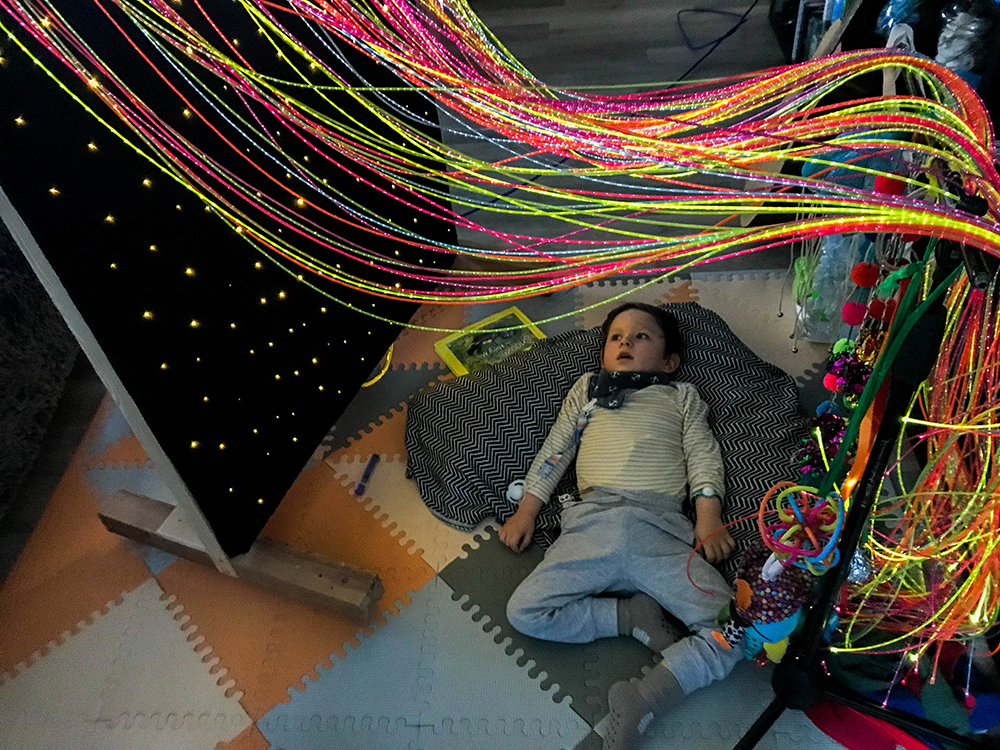
And now Mikaere has a gait walker. It’s beautiful. He’s tolerating it for longer and longer periods (it helps that his vision has improved and he now watches TV. The walker puts him at the right height). He doesn’t throw his head back anymore, and has learnt to hold his head forward (which means we don’t need to hold his head!). He’s beginning to understand the concept of taking steps (with a lot of support, not independently!) but mostly, he’s feeling his legs and his ankles upright, free of straps. He moves his legs, moves his ankles, and that’s everything. He also smiles when he’s in it, which is everything.
So, onwards we go. Upright, with feet free. With Disco parties in the hallway. We’re doing it!