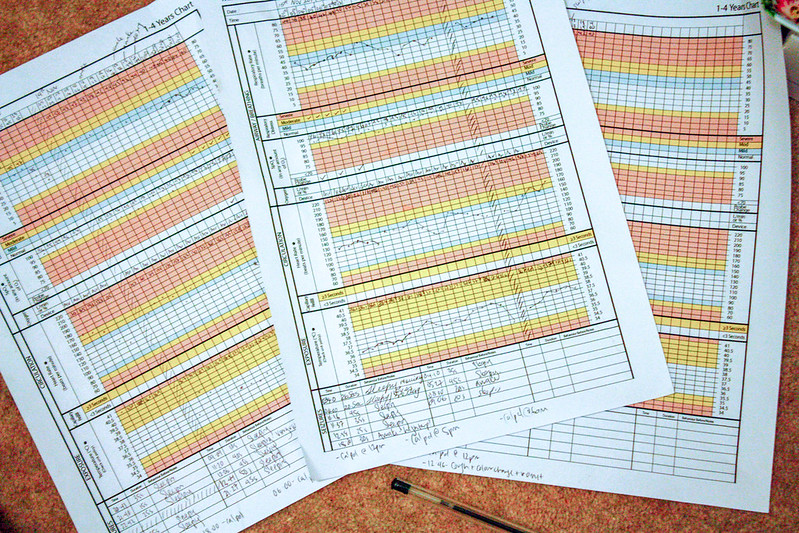
Mikaere’s had the once over by several people. His nurses have taken bloods, he’s had a nebuliser and is on o2. His gas and air look good (his lactates especially), his temp is holding steady and we had a visit from a PICU Nurse we know who came in to say hey.
So no red giant flags, and I have a chance between consultants to go get breakfast.
And as I’m walking down the familiar halls to M&S I think Saturdays are the best days to be here. There are less people in the hospital today. We had the bonus of coming in early, just after the shift change but before all the other kids had enough time to hurt themselves and fill up the a&e waiting room.
Is it weird that I think all this? That I know the time shift change happens? That I know when the lulls and peaks of our a&e are? That I come armed with a cheat sheet that answers 99% of the nurses/drs questions, and the two questions I’m asked (what is blood test for glycine on the system as – amino acid blood profile – and what colour is the bottle – green) – I can answer without really thinking about.
Our last a&e visit was months ago. MONTHS ago. I guess this is the winter season kicking off, right after a week of appointments and therapies after the summer break. I’m not happy we’re here, but now that we are I’m not panicking about it, too much. I’m hopefully we’ll make it home this afternoon sometime.
—-
A few hours later and I’m worried. We’re still in the A&E majors, Mikaere’s still on o2 and sleeping, but he’s not holding his o2 levels above 92%. We need 94% or higher. We up the rate to 1L. That’s the borderline dose. It’s not a super high dose of o2… but any higher and we’re staying over.
The nurse notes say they’ve booked a bed upstairs on the ward (just in case) and I’m positive that if this was any other kid, or if I hadn’t expressed my concerns about the risks of being on the ward we’d be up there already for observation rather than down here. But down here is safer. Down here the A&E majors is filled with broken bones and a girl with ENT drama. There are no other chest infections or mystery illnesses in our room. The ward I know is probably filled with more things that pose a risk.
So we wait, we see. The idea is that the longer on o2 he is the easier it’ll be for him. His body won’t have to work so hard, he’ll have more in the tank for recovery. Or so we hope.
I’m worried though. I don’t want to go up to the ward. That’s the start of the path towards deterioration and I’m scared that each escalation will mean a step toward terminal.
But we’re not there yet. We’re not. We’re just in A&E still, just in observation. We’ll see.
—-
The bloods are back. The chest xray clear. But Dr Erin has a game plan. She called our apartment a mini hospital. We have suction, a stat monitor and oxygen. We have all the medical equipment that Mikaere’s currently making use of on A&E.
I think that’s our saving grace. Kai’s just barely managing to keep his stats up with o2, and we’re able to wean to 0.5L when he’s awake. It’s a small wean, but it’s enough. We’re discharged with very strict instructions of what to look for and when to come back. We have nurses calling to check in, and with a discharge note we’re waved off.
Mikaere’s not any better than he was this morning, but he’s not any worse. I was right to put him on o2 it turns out + I’m grateful for the reassurance.
Kai’s ill. He’s not holding his o2 levels up by himself. But we’re home. Thank fuck for that.