There’s an appointment I always dread and it happened last week. We met with our palliative care consultant at Hospice. She’s really lovely, has a keen sense of humour and is generally very sympathetic. She’s also incredibly practical and straightforward which I enjoy.
It wasn’t our palliative care consultant that made me dread this appointment, though. It’s that every six to nine months (acute events or slow declines not withstanding) we review Mikaere’s end of life care plan. Which is to say we go through, step by step and say, if the worst case scenario happened – at what point do we say enough is enough.
Blah. Just BLAH. My son is beautiful and right this minute chirpy and smiley and very happy kicking the crap out of some shredded paper. I hate having emotionally to go to that dark place. To remember the time he turned blue, that time he was in a seizure coma and then really think about his quality of life and the quality of death we’d wish for him. I hate that bit too. Thinking about his death. I mostly block out that it’s a very real and likely possibility. It just seems so unlikely because he’s so beautiful and alive and aware and happy. But mostly because I don’t want it to happen. It seems unlikely because I don’t want it to happen.
But then I think about to Halle Mae who gained her wings only a few months ago. I think about all the NKH babies who have passed and I know for certain it’s a possibility. And if it’s a possibility, then having a plan when we’re not in the world of grief, having something to fall back on and not have to make those decisions when we’re emotionally struggling is a good idea.
But to have a plan we have to consider the worst case scenario and I hate the worst case scenario. Even worse, this time it was just me. Sam had to work, so there I was. Our palliative care consultant, a palliative care nurse, our carer and a lady shadowing palliative care in hospice (because the more the merrier, apparently). A whole panel of people.
And we went down the list.
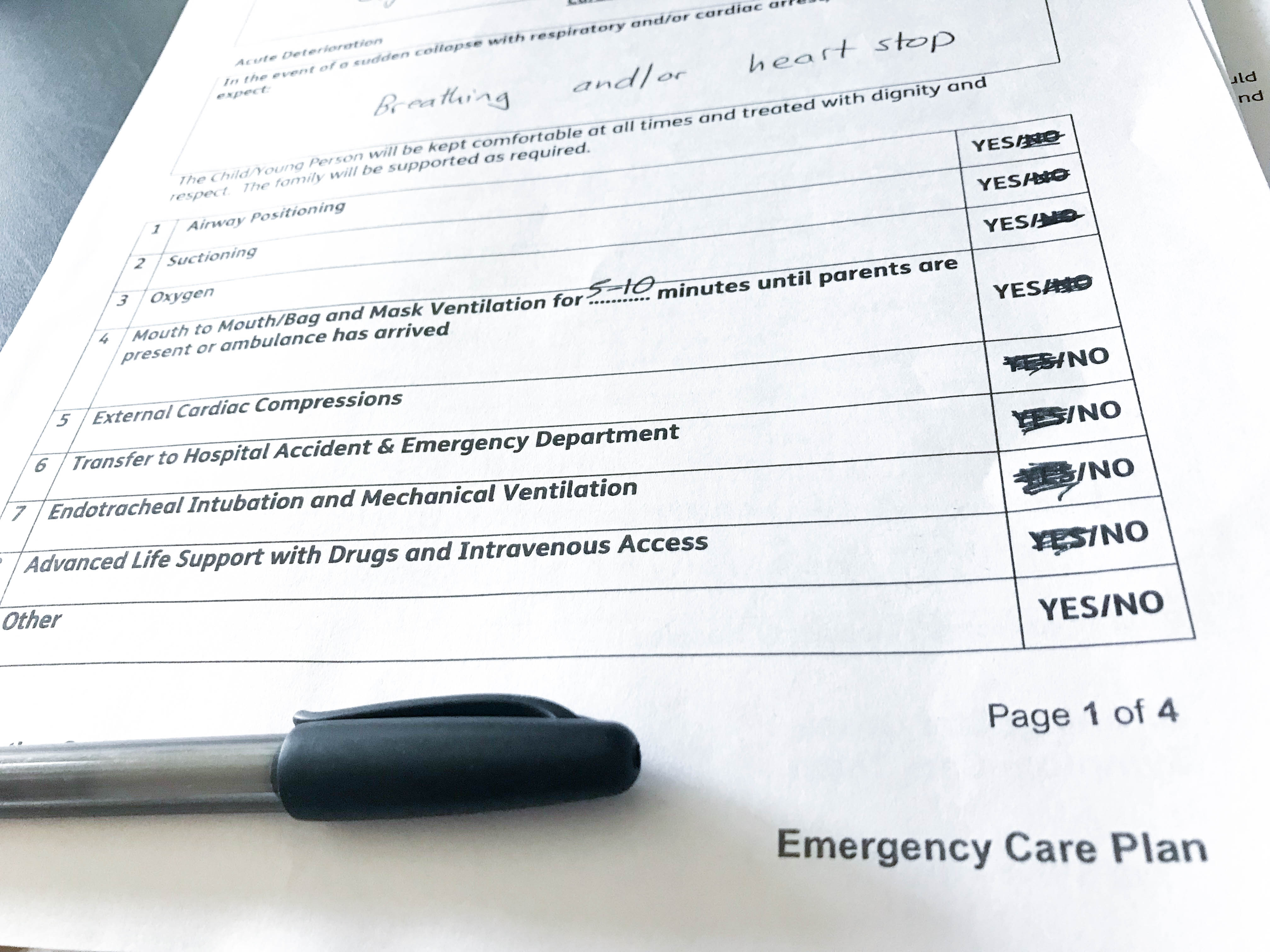
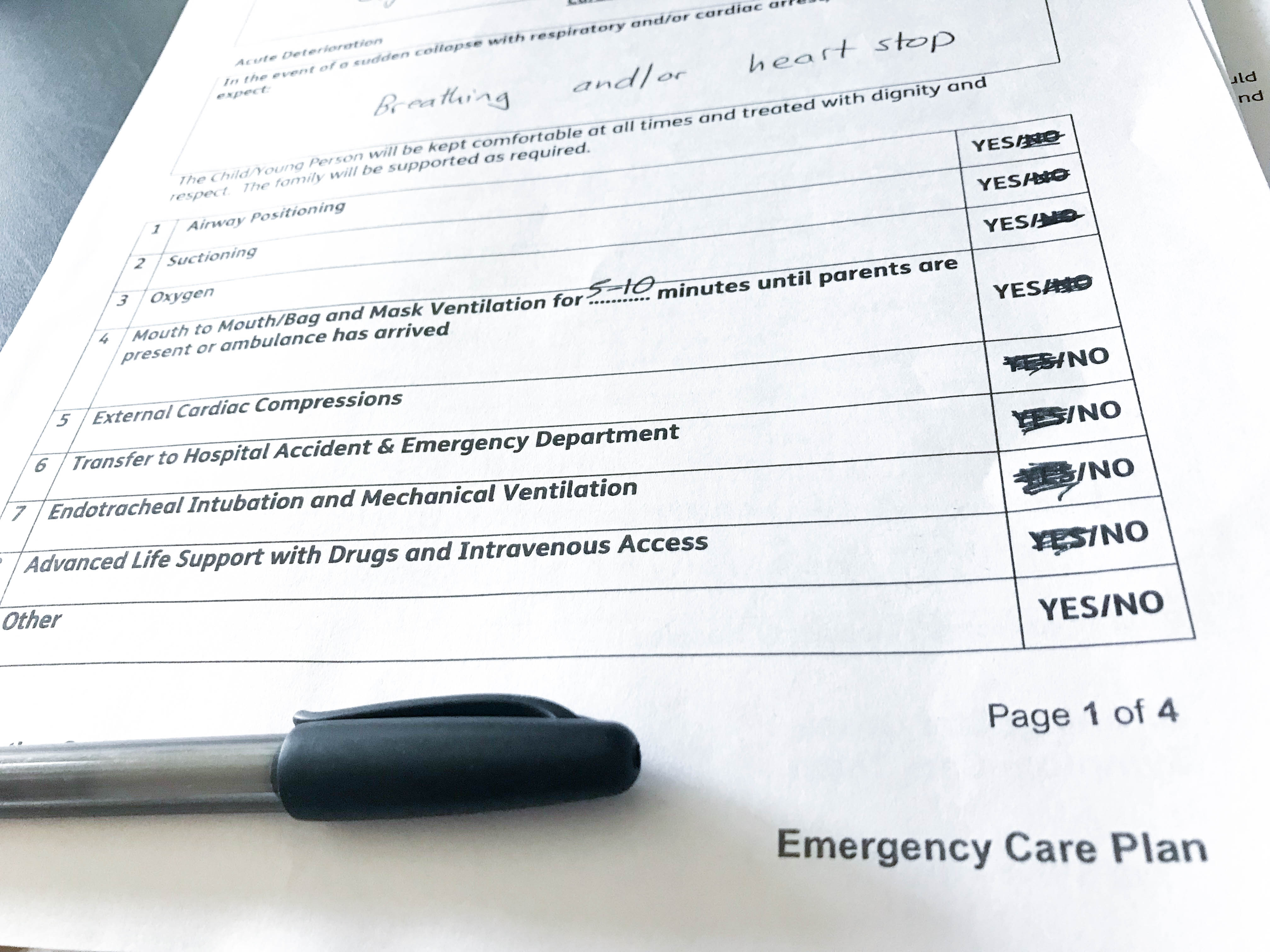
Our first scenario is an acute deterioration, which is to say “in the event of a sudden collapse with respiratory and/or cardiac arrest, where breathing and/or heart stops, we agree to”:
(it starts from the least invasive treatments)
- Airway positioning. Yes. Do this. Reposition his airway, for sure.
- Suctioning. Also yes. If we can get him breathing again with suction, it would be silly not to.
- Oxygen. Yes. Yes to O2 through a nasal cannula.
These ones are all easy ones. They don’t hurt, they’re temporary and won’t cause any long term damage. The next one is:
- Mouth to Mouth/Bag and Mask Ventilation for _____ minutes until parents are present or ambulance has arrived.
We said yes. For 5-10 minutes. And we debated every single one of those minutes, and the whys and whats and all the scenarios. It was hard not to say you do mouth to mouth for as long as you need to. It was hard to find the point to let go and that 5-10 minutes is our point. I even called Sam, interrupting his work day to help talk it out.
Because the next one?
We said no to External Cardiac Compressions.
We said no to CPR. I hate that we said no, but thinking about whats best for Mikaere rather than whats best for my emotional state… it’s a no. With a child, cardiac arrest is typically caused by respiratory arrest (the opposite is true in adults). Which is to say, if Mikaere has stopped breathing for long enough, it’s likely to also stop his heart from breathing.
If his breathing had stilled for long enough that his heart stops beating despite our interventions that’s a big big problem, cardiac compressions are likely to break his ribs and he’s still unlikely to survive. Quality of death. That’s what I keep telling myself. Quality of death is just as important as quality of life.
The rest? They were easy to say no to.
- No to Endotracheal intubation and technical ventilation.
- No to advanced life support with drugs and intravenous access.
No thank you. We’ve been there before, with both those scenarios. And considering the quality of life following those scenarios… we genuinely feel it would be better for Mikaere to pass. Quality of death, quality of life.
This scenario was by far the worst one. The acute deterioration, where it happens swiftly and unexpectedly. The other scenario, a slow deterioration instead of an acute event we’d be able to see it coming. It would be increased seizures, reduced consciousness, and Mikaere would increasingly be struggling to maintain his airway.
In this scenario, we’d do everything we could, up until intravenous access (with still no to mechanical ventilation). But with a slow deterioration, we’ll have the time to consider what’s best. We’ll have time to think on whether each intervention is right. The main point here is that we’d be able to transfer to hospice on end of life care if need be. There isn’t a point where we’d say we want to go to hospice. If it was anything like last time, we’ll all know it’s time. We’ll have the support we need to decide what’s best for Mikaere.
To be fair, we can change our minds at anytime about anything on the plan. We’re not locked in, but I think if it happens it’s best to have a plan. I know how crazy it gets, how fast everything moves and how you can get into a knee-jerk reaction only mode. How you can be so overwhelmed with all your feelings that thinking logically isn’t possible. That we might be still processing our fear and our grief to clearly think about whats best for for Mikaere.
Still, I walked out of the room heavy. So so heavy. It was beautiful day and Mikaere was happy, but it was a really really tough day. I’m glad we have a plan to which we agree on, but I hate we even need a plan. I hate NKH, I hate that we’re planning for his death. It’s horrific.
So, a cure, hey? That’s what we need. I’m thinking on more fundraising opportunities – because that’s what gets me through, and that’s what gives me hope. Wine tasting later in the summer – what do you think? Anyone keen?